Type 2 Diabetes Prevention Week 2021

Date
Location
Search Awareness Days
What is Type 2 Diabetes Prevention Week?
Type 2 Diabetes Prevention Week is a nationwide annual campaign in the UK that aims to raise the awareness of Type 2 diabetes and ways to prevent it. This year it will be held from Monday-Sunday, 10-16 May 2021.
Launched in 2018 the campaign provides toolkits, posters, leaflets, bunting, waist tape measures, stickers, animation clips, promotional videos, social media and digital resources. Clinical Commissioning Groups and GPs are encouraged to take part, and roadshows are conducted around the country especially targeting at-risk groups.
It also helps promote an NHS programme called “Healthier You: NHS Diabetes Prevention Programme” – a free service from NHS England, Public Health England, and Diabetes UK for people at high risk of Type 2 diabetes. It provides advice on healthy eating, being more active and managing weight through a face-to-face sessions and a digital version of the service.
There are approximately 3.9 million people in the UK living with diabetes and a further 900,000 who likely have it but haven’t yet been diagnosed bringing the total to 4.8 million. Put another way, one in 15 people in the UK now live with diabetes.
There are two main types of diabetes. Type 2 which represents about 90% of cases, and Type 1 a further 8%. Type 2 is by and large preventable and has a terrible toll on people’s health and wellbeing. According to Diabetes UK:
- Each year in the UK, 24,000 people with diabetes die early
- Diabetes is the leading cause of blindness in people of working age in the UK
- Over 100 amputations are carried out every week on people with diabetes because of complications connected with their condition. Up to 80 per cent of these are preventable
It also has a terrible impact on the National Health Service. The Charity also estimated that in 2010 the cost of diabetes to the NHS was approximately £10bn per year. This was estimated to rise to £16.9bn by 2035/36.
The Week is not to be confused with Diabetes Week, Hypo Awareness Week or Insulin Safety Week in the UK, World Diabetes Day or American Diabetes Month, .
As a Type 1 diabetic myself I take a particular interest in this campaign.
What is Diabetes?
Diabetes is a condition where the body can’t naturally control the amount of glucose (sugar) in the blood. Blood sugar levels rise and in turn cause medical complications.
Glucose is the main source of energy we need to function (run, walk and go about our daily lives). It is produced by the food we eat mostly through carbohydrates like bread, pasta, rice, potato, sweets and chocolate.
However, to be used as energy glucose needs to pass through the digestive system and enter the body’s muscles and cells via the bloodstream. This transition of insulin from the blood to the cells is enabled by a hormone called insulin which is produced by the pancreas.
If the pancreas doesn’t produce enough insulin or we become resistant to it, glucose will remain in the blood and cause blood sugar levels to rise.
The body’s inefficient use of insulin, a resistance to it or when the pancreas has packed up altogether is the cause of diabetes and it can cause serious health problems as we discuss below.
What are the Symptoms of Diabetes?
Symptoms of diabetes are typically:
- Thirst
- Weight loss
- Tiredness
- Urinating often
- Itchy private parts
- Cuts and wounds taking a long time to heal
- Blurred vision
I recall I had many of these symptoms when I was diagnosed. I was working in Southeast Asia at the time but given the hotter climate thought little of feeling thirsty despite drinking water like it was going out of fashion. I was terribly tired for two or three weeks and would just want to go to sleep in the afternoon.
I went to the doctor and to my surprise had lost heaps of weight too: down from my usual fighting weight of around 80kgs to a mere 68kgs.
Note: having these symptoms does not mean you are necessarily diabetic. If you’re concerned, you should see a doctor.
How to Test for Diabetes?
Testing for diabetes is straightforward and typically involves a blood or urine test. What they test for is different in each case:
- C-peptide: finds out how much insulin your body is producing
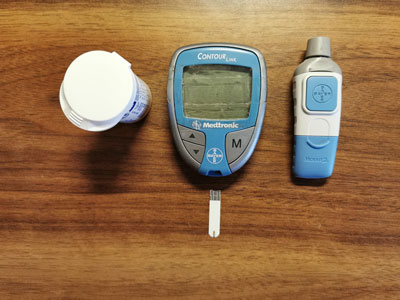
- Fasting Plasma Glucose Test: this is the finger pricking test you see diabetics do on a daily basis. Also called a ‘fasting blood sugar test’ it requires the patient not to eat for 8-10 hours prior
- GAD Antibodies Test: to discover whether someone has either Type 1 diabetes or Latent Autoimmune Diabetes of Adulthood (LADA)
- Oral Glucose Tolerance Test: can help diagnose instances of diabetes mellitus or insulin resistance
To complicate things slightly more you’ll see two measurements used with blood glucose test results:
- MMOL/L or millimoles per litre: international standard and used in the UK
- MG/DL or milligrams per decilitre: used in USA, Germany and elsewhere
The National Institute for Health and Care Excellence (NICE) recommends target blood glucose levels as below alongside the IDF’s target ranges for people with diabetes:
| TARGET LEVELS | BEFORE MEALS (PRE PRANDIAL) | 2 HOURS AFTER MEALS (POST PRANDIAL) |
| No diabetes or in health | 4.0 to 5.9 mmol/L (72-106 mg/dl) | Under 8 mmol/L (144 mg/dl) |
| Adult with Type 1 diabetes | 4 to 7 mmol/L (72-126 mg/dl) | Under 9 mmol/L (162 mg/dl) |
| Adult with Type 2 diabetes | 4 to 7 mmol/L (72-126 mg/dl) | Under 8.5 mmol/L (153 mg/dl) |
| Children with Type 1 diabetes | 4 to 8 mmol/L (72-144 mg/dl) | Under 10 mmol/L (180 mg/dl) |
Diabetes Facts, Figures and Statistics
Diabetes is one of the fastest growing, preventable medical conditions in the world.
United Kingdom
Diabetes is growing at a worrying rate in the UK. According to results from the 2017 National Diabetes Inpatient Audit, around one in six hospitals beds are occupied by a person with diabetes. According to Diabetes UK the prevalence of diabetes in the UK in 2019 was 3.9 million, i.e. the number of people already diagnosed; 90% of diabetics are Type 2 and 8% Type 1:
| Prevalence | 2018-2019 |
| England | 3,319,266 |
| Northern Ireland | 99,833 |
| Scotland | 301,523 |
| Wales | 198,883 |
| UK | 3,319,505 |
There are believed to be a further 900,000 people though living with diabetes who have not yet been diagnosed bringing the total to 4.8 million.
Some headline statistics include:
- At least 10,350 people in the UK have end stage kidney failure because of their diabetes
- More than 1,700 people have their sight seriously affected by their diabetes every year in the UK
- Every week diabetes leads to more than:
- 169 amputations. Someone with diabetes is 20 times more likely to experience an amputation than someone without diabetes
- 680 strokes
- 530 heart attacks and almost 2,000 cases of heart failure
- More than half of all cases of Type 2 diabetes could be prevented or delayed
- Obesity is responsible for 80 to 85% of someone’s risk of developing Type 2 diabetes
- The NHS spends at least £10 billion a year on diabetes. That’s 10% of its entire budget
- One in six people in a hospital bed has diabetes
- In some hospitals over a quarter of beds are used by people with diabetes
- People with diabetes are twice as likely to be admitted to hospital
- Almost 80% of the money the NHS spends on diabetes is on treating complications
And the list goes on.
Worldwide
While the condition used to be associated with the ever-growing waistline of Western and developed nation countries major health associations including the World Health Organisation now see it as a global problem, especially one affecting middle to lower income countries.
To quote the International Diabetes Federation:
- Approximately 463 million adults (20-79 years) were living with diabetes; by 2045 this will rise to 700 million
- The proportion of people with Type 2 diabetes is increasing in most countries
- 79% of adults with diabetes were living in low- and middle-income countries
- 1 in 5 of the people who are above 65 years old have diabetes
- 1 in 2 (232 million) people with diabetes were undiagnosed
- Diabetes caused 4.2 million deaths
- Diabetes caused at least USD 760 billion dollars in health expenditure in 2019 – 10% of total spending on adults
- More than 1.1 million children and adolescents are living with Type 1 diabetes
- More than 20 million live births (1 in 6 live births) are affected by diabetes during pregnancy
- 374 million people are at increased risk of developing Type 2 diabetes
The Federation also lists and projects the top 10 countries (in millions) with the highest number of people with diabetes:
| Country | 2019 | Country | 2030 | Country | 2045 |
| China | 116.4 | China | 140.5 | China | 147.2 |
| India | 77 | India | 101 | India | 134.2 |
| USA | 31 | USA | 34.4 | Pakistan | 37.1 |
| Pakistan | 19.4 | Pakistan | 26.2 | USA | 36 |
| Brazil | 16.8 | Brazil | 21.5 | Brazil | 26 |
| Mexico | 12.9 | Mexico | 17.2 | Mexico | 22.3 |
| Indonesia | 10.7 | Indonesia | 13.7 | Egypt | 1639 |
| Germany | 9.5 | Egypt | 11.9 | Indonesia | 16.6 |
| Egypt | 8.9 | Bangladesh | 11.4 | Bangladesh | 15 |
| Bangladesh | 8.4 | Germany | 10.1 | Turkey | 10.4 |
Most countries with the highest percentage figures are island nations. In 2019 these were:
| Country | Prevalence % |
| Marshall Islands | 30.5 |
| Kiribati | 22.5 |
| Sudan | 22.1 |
| Tuvalu | 22.1 |
| Mauritius | 22 |
| New Caledonia | 21.8 |
| Pakistan | 19.9 |
| French Polynesia | 19.5 |
| Solomon Islands | 19 |
| Guam | 18.7 |
Types of Diabetes
There are in fact several types of diabetes. However, there are two main types which cover 98% of people with the condition in the UK. How diabetics manage their diabetes depends on which type they have.
Type 1 Diabetes
Type 1 diabetes is what’s known as an auto-immune disease: the body attacks and destroys the cells in your body that make insulin. In effect, your pancreas has packed up.
Type 1 diabetes is also typically inherited from parents (my father is Type 1 as well) though there are instances, albeit less common, where there is no family history of it.
As the pancreas has stopped working Type 1 diabetics need to inject insulin several times a day to literally stay alive. Not injecting insulin would mean constantly high blood sugar levels which would have disastrous effects on health (see below).
How often you inject and what type of insulin you inject will depend on the way the insulin is administered.
There are two types of insulin:
- Basal: also known as background insulin, basal insulin is long acting and works for approximately 12-24 hours to counteract the natural production of sugar your body makes. One or two injections are required every day
- Bolus: an injection taken with every meal to counteract the carbohydrates eaten. Three or more injections are required per day
There are two methods of administration. Type 1 diabetics use one or the other, not both:
- Insulin pen: a pre-filled insulin cartridge in a pen-like dispenser (see image below). Note the pens are different: the orange is the bolus, the green is the basal
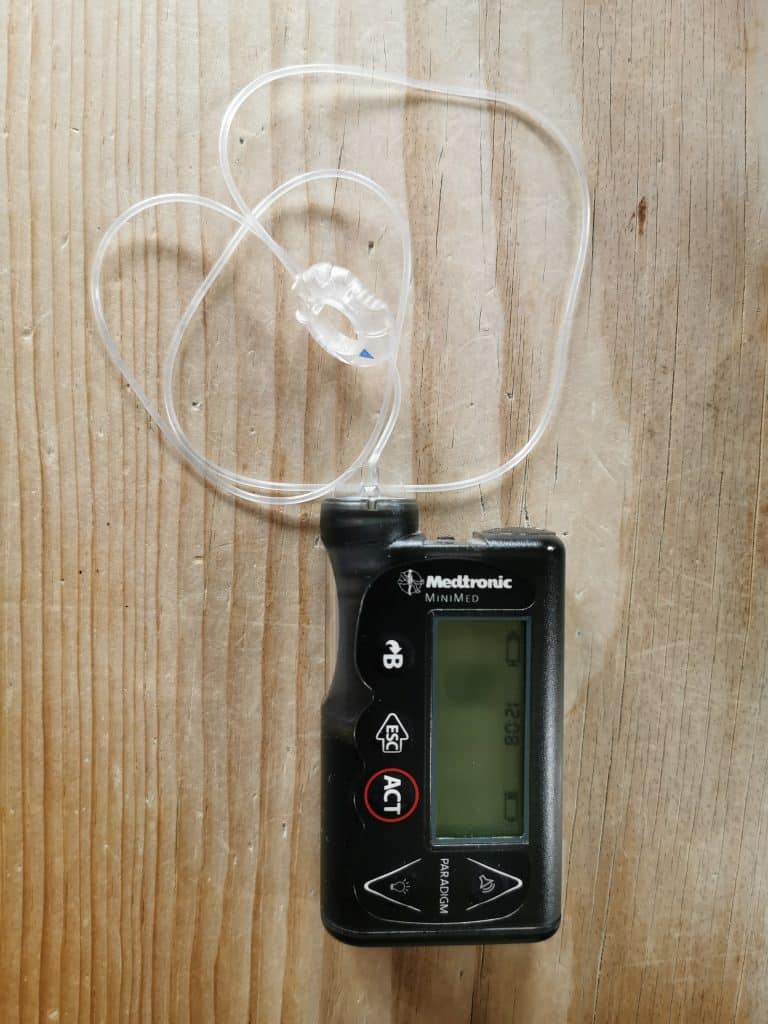
- Insulin pump: a little machine the size of a computer mouse attached to the body via an adhesive patch. The pump dispenses the same insulin the whole time: at a specified rate per hour for the basal throughout the day, and with each meal for the bolus (you need to press a few buttons yourself to do this). It consists of the pump, a reservoir of insulin and an infusion set. When the reservoir runs out or the adhesive patch loses its stickiness you prepare a new one and reattach it to the body
How much insulin you inject depends on the type and quantity of food we eat, your resistance to insulin, and the amount of exercise you do: more carbs = more insulin, less carbs = less insulin, but one’s resistance to insulin varies from person to person.
I, personally, use a pump which is a fantastic piece of kit.

Type 1 diabetics are also often prescribed statins.
Managing Type 1 diabetes can be complicated and it takes time getting to grips with. There is nothing you can’t eat but you should eat and drink in moderation and of course do regular exercise.
‘Going low’, when the blood sugar level drops below 4 mmol/l (72 mg/dl) and you start to feel light-headed, is a common occurrence for Type 1 diabetics (see hypoglycaemia below) as is being ‘too high’ (see hyperglycaemia). Keeping within the ranges in the table above are important.
Exercise rapidly brings down the sugar level and is a common cause of people going low as well, especially unplanned exercise.

Once you’ve got to grips with it though, I know from personal experience and the health experts will confirm this, if you manage the condition properly there is little you can’t do.
For example, I’ve completed an Ironman triathlon, ridden 100-mile bike rides, completed half-ironman and Olympic distance triathlons, and done a 5km Swimathon (raising perhaps £3,000 for Diabetes UK in the process). You’re most welcome to follow me on Twitter as Type1Rob or visit my website Diabetes and Exercise (a shameless plug I admit but I’m not terribly active on there).
Another Type 1 chap I know, virtually at least, is Roddy Riddle. He’s completed various Ironman triathlons, the Marathon des Sables, and walked across the North Pole to name a few of his achievements.
My point is to illustrate that having Type 1 diabetes shouldn’t hold you back from doing what you enjoy. You’ll find many famous people with diabetes. Just take precautions, prepare properly and you’ll be fine (I have blood glucose testing meters at home, the office, in the car and my sports bag along with a supply of dextrose tablets).
Type 2 Diabetes
Type 2 diabetes is by far the most common type and affects 90% of all diabetics in the UK. It is typically caused by a poor diet, lack of exercise or advancing age though some ethnic groups are particularly susceptible. The pancreas still works with Type 2s but the body has become resistant to the insulin it produces.
You’re more likely to have Type 2 if you:
- Are overweight or obese
- Have an immediate family member with type 2 diabetes
- Are over age 45
- Are physically inactive
- Have ever had gestational diabetes, which is diabetes during pregnancy
- Have given birth to a baby weighing more than 9 pounds
- Are African-Caribbean, Black African, or South Asian
- Have polycystic ovarian syndrome
- Have a lot of belly fat
Symptoms are very similar to those of Type 1.
While many Type 2 diabetics will be prescribed metformin a few also need insulin but an improvement in lifestyle and diet are the best medicines. Some people may also go into remission. Diabetes UK say this is most likely to happen nearer the time of diagnosis and is strongly linked to weight loss but there is still no cure for the disease as the condition can always return.
Medical Problems Associated with Diabetes
Diabetes affects people physically but also mentally given the lifestyle changes they often have to make.
According to Diabetes.co.uk, diabetes is currently the fifth most common reason for death in the world:
- Around 1 in 8 people between 20 and 79 years old have their death attributed to diabetes and it is expected to rise
- The life expectancy on average now is reduced by:
- More than 20 years for people with Type 1 diabetes
- Up to 10 years for people with Type 2 diabetes
Hypoglycaemia
Hypoglycaemia is especially common in people with Type 1. Also known as a ‘hypo’ or ‘going low’ it is caused when the blood sugar level drops below 4mmol/l (72mg/dl). Symptoms include having zero energy, feeling anxious, light-headed, hungry, irritated (more than usual!), and getting sweaty or clammy hands.
In the most part you can deal with these symptoms yourself by consuming fast-acting sugar like fruit juice, dextrose tablets or a sugary snack but it’ll take 10-15 minutes to work so sit down and just relax! As soon as you feel better take a more long-lasting carbohydrate like a piece of toast or a meal.
In the worst cases you could appear as though you are drunk, you could collapse or become unconscious in which case you need immediate medical attention either with a shot of glucagon or by calling 999.
Hypos tend to happen after missing a meal, giving yourself too much insulin, unplanned exercise or boozing on an empty stomach.
Type 1 diabetics can also get hypo anxiety: the fear of going low when out and about and not being able to control the outcome.
Type 1 diabetics only have three year driving licenses as well after which it needs renewing and a medical questionnaire completing telling the authorities of any hospitalisation or regular hypos. Clearly, we don’t want people going low at the wheel.
Type 1 diabetics also need an annual eye test to identify diabetic background retinopathy, and a foot test to test for blood circulation problems and sensitivity.
Hyperglycaemia
Hyperglycaemia is when sugar levels rise too high. What is too high? Well, it varies from person to person but Diabetes UK states usually above 7 mmol/l (126 mg/ml) before a meal and above 8.5 mmol/l (153 mg/dl) two hours after.
Symptoms include thirst, frequent urinating, tiredness, stomach pain, feeling sick or breath that smells like pear drops.
It is generally caused by missing an insulin dose, not taking enough insulin, overeating, being stressed, having a fever or cold, or lack of exercise.
Being ‘high’ once in a while won’t cause interminable damage but if it occurs regularly or your blood sugar is over 20-30mmol/l then there is cause for immediate concern in the form of Diabetic Keto Acidosis (DKA) or more long-term effects such as damage to the eyes, nerves, kidneys, heart and blood vessels and more.
If you’re Type 1, immediate treatment for a simple high blood sugar level can be given with a dose of insulin. If you’re feeling really unwell or if it happens regularly you’ll need to change your insulin regime, diet, exercise routine and speak to a doctor.
Diabetic Keto Acidosis (DKA)
Diabetic Keto Acidosis or DKA is a serious complication that affects Type 1s and some Type 2s, and can result in coma or even death if not treated quickly.
It is caused by a build up of ketones in the blood that quickly become acidic.
Other Medical Problems
Diabetics are likely to be diagnosed with more medical problems than the average man or woman.
Compared to people without diabetes, people with diabetes are more than 2.5 times more likely to experience heart failure, nearly 2.5 times more likely to have a heart attack, 2 times more likely to have a stroke.
This is more worrying for Type 1 diabetics. Compared to people without diabetes, people with Type 1 diabetes are 4.5 times more likely to experience heart failure,more than 4 times as likely to have a heart attack, and 3.5 times more likely to have a stroke.
Diabetes leads to more than 8,500 leg, toe, or foot amputations every year. Someone with diabetes is 20 times more likely to experience an amputation than someone without diabetes. That’s more than 160 a week.
More than 1,700 people have their sight seriously affected by their diabetes every year in the UK. Diabetes is one of the leading causes of preventable sight loss in the UK.
At least 10,350 people in the UK have end stage kidney failure because of their diabetes. More than one in three people who need kidney dialysis or a transplant have diabetes. People with diabetes are five times more likely to need either kidney dialysis or a kidney transplant.
… among other problems.